Patient-centricity isn’t a slogan — it’s the operating model for launch, access, adherence, and real-world outcomes. Regulators have elevated the patient voice (FDA’s Patient-Focused Drug Development), nationwide exchange is accelerating via TEFCA, accessibility is measurable against WCAG 2.2, and experience is tracked with CAHPS. Teams that operationalize consented data, inclusive design, and outcome-based KPIs move faster and prove value — without tripping compliance.
How Pulse helps: Pulse Health unifies consent capture, role-based access, journey orchestration, multilingual messaging, analytics, and audit trails — so patient-first programs actually ship.

What “patient-centric” really means
Patient-centric pharma marketing treats the patient’s needs, constraints, preferences, and context as the blueprint for everything — not a post-hoc add-on. It blends empathy (plain language, transparency), shared decision-making (supporting conversations among patients, caregivers, and HCPs), inclusivity (language, culture, health literacy), and privacy-by-design. The business case: faster time-to-therapy, higher first-fill and persistence, and better patient-reported outcomes (PROs) — because people understand, can afford, and can follow therapy.

How Pulse helps: Persona builder + journey templates map needs, barriers, and preferred channels (SMS, email, portal, chat), then route communications and human handoffs accordingly.
Transition: If patient-centricity is the “what,” the “why now” is policy, data, and measurement maturing at once.
Why the shift is inevitable (policy, tech, measurement)
- Policy: FDA’s PFDD guidance elevates patient input across development and evaluation.
- Interoperability: TEFCA is enabling network-to-network data exchange at scale.
- Accessibility: WCAG 2.2 sets concrete standards for inclusive digital content.
- Experience measurement: CAHPS normalizes patient-experience KPIs.
- Evidence: FDA is expanding the role of real-world evidence and codifying PRO use in trials and labeling (e.g., oncology’s core PRO set).

How Pulse helps: Interoperable integrations blend consented data into journeys; dashboards tag PROs and experience metrics to program changes.
Transition: With the “why” settled, here’s the practical “how.” Start with six pillars you can implement in 90 days.
The six pillars of patient-centric pharma marketing
1) Consent & data governance by design
Bake privacy into the journey: explicit consent flows, Business Associate Agreements, role-based access, audit trails — and alignment to the HIPAA Privacy/Security Rules and 21 CFR Part 11 for trustworthy e-records/signatures.

How Pulse helps: Prebuilt consent ledger; role-based access; immutable audit logs; approval workflows with redlines and versioning.
2) Needs-based segmentation
Move beyond demographics to segment by health literacy, language, SDOH barriers, digital comfort, care-team dynamics, and affordability. Use these inputs to tailor cadence, channel, and content — especially around benefits verification, prior-auth, and copay/PAP navigation.
How Pulse helps: Persona builder captures literacy/language/SDOH signals; affordability modules and live-agent handoffs.

3) Omnichannel journeys, accessible by default
Orchestrate SMS, email, portal, live chat, and human support. Optimize flows for screen readers, tap targets, focus order, and transcripts — then test against WCAG 2.2.

How Pulse helps: WCAG-aware templates; QA checklists; multilingual variants and low-bandwidth modes.
4) Education that empowers
Deliver plain-language content when decisions happen (post-visit, post-denial, refill windows): side-effect coaching, step-by-step PA guidance, and cost options.
How Pulse helps: Triggered nudges; reusable content for adverse-event coaching; benefits investigation updates.
5) Community & trust
Partner with advocacy groups; enable moderated peer support; align language with National CLAS Standards for culturally and linguistically appropriate services.

How Pulse helps: Language routing, interpreter workflows, micro-community modules with moderation tools.
6) Outcome-focused measurement
Track the metrics that matter: time-to-therapy, first-fill rate, 90-day persistence, PRO deltas, and experience measures aligned to CAHPS. Use these to iterate journeys and investment.
How Pulse helps: Out-of-the-box KPI packs, cohort comparisons, and ROI calculators.

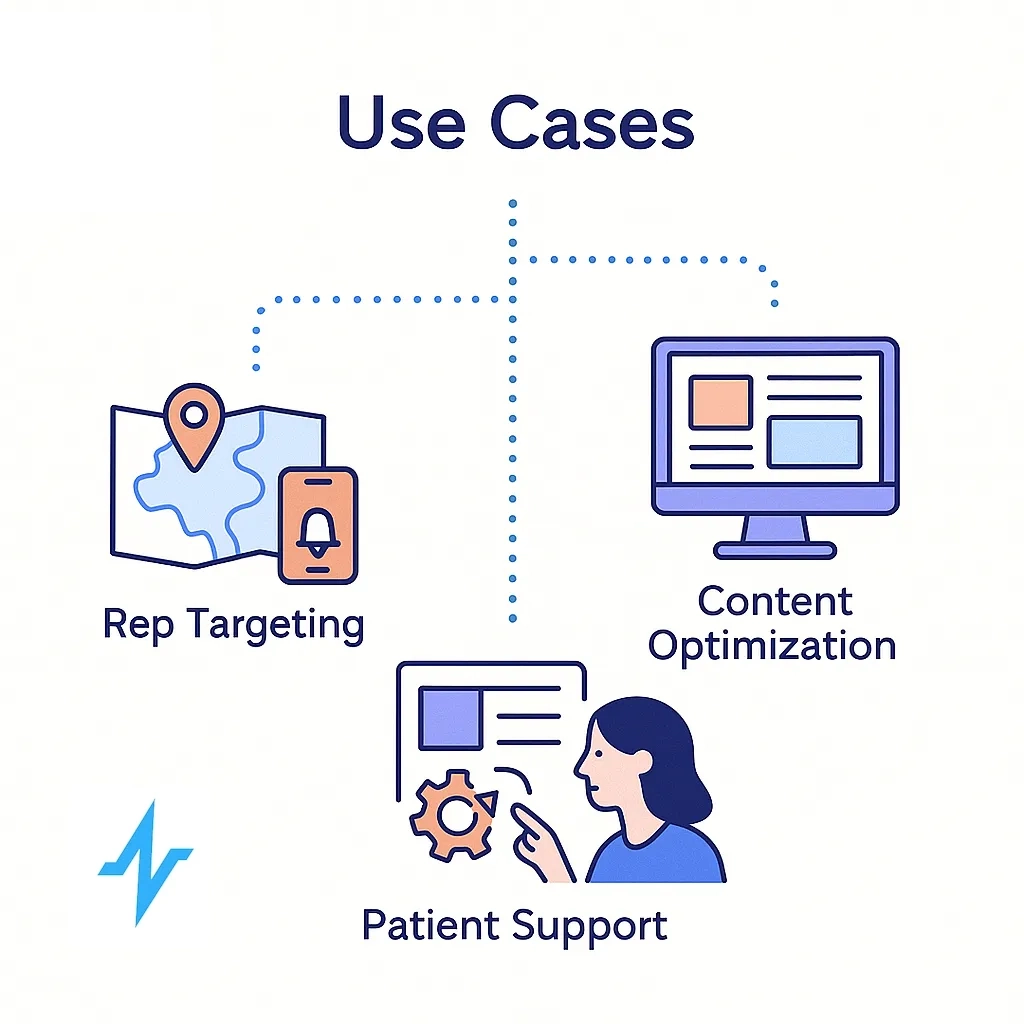
Use cases across the product lifecycle
Pre-launch. Build patient insights, map journeys, and design inclusive clinical-trial outreach. Modernize consent via eConsent and plan for eCOA/PRO collection. Where appropriate, incorporate decentralized elements per FDA’s DCT guidance.
Launch. Smooth access with onboarding, PA support, affordability (copay/PAP), and side-effect education — sequenced to remove friction at each step.
Post-launch. Improve persistence with refill reminders, symptom tracking, registry enrollment, and RWE generation aligned to FDA’s RWE program.
How Pulse helps: Libraries for onboarding/adherence, registry connectors, and PRO tagging that feed outcomes dashboards.
Transition: Being “patient-first” also means for everyone — equity and accessibility aren’t optional extras.
Equity & accessibility (design for all)
Use the National CLAS Standards to guide culturally/linguistically appropriate services and content. Build every artifact to WCAG 2.2 — alt text, captions/transcripts, keyboard navigation, readable typography, and low-bandwidth options to reduce digital divide friction.

How Pulse helps: Translation memory, interpreter routing, WCAG checklists, and templated accessibility QA.
Tech & data architecture (what sits under the hood)
Use a HIPAA-ready CRM as your orchestration layer; integrate EHR/claims/hub/PBM data via HL7 FHIR and connect to national exchange under TEFCA (see the ONC/RCE FHIR Roadmap for TEFCA Exchange). Secure operations with HIPAA safeguards and ensure records/signatures meet 21 CFR Part 11 where applicable.
How Pulse helps: Secure APIs; consent ledger; role-based access; MLR routing with SLA timers, side-by-side redlines, and immutable audit trails.

Governance & MLR that doesn’t slow you down
Stand up a RACI, reusable checklists, and documented approvals with expiry/recertification. “Shift-left” compliance by embedding privacy, medical, legal, and regulatory requirements into drafting and review. For a practical playbook, see Navigating Compliance in Pharma CRM & Communications and Data Privacy in Pharma Marketing.

KPIs and a simple 90-day pilot plan
KPIs: time-to-therapy (TtT), first-fill rate, 90-day persistence, PRO deltas, and patient-experience metrics aligned with CAHPS.
Pilot (12 weeks):

- Pick one condition + two personas;
- Stand up consented, WCAG-aligned journey;
- Benchmark KPIs;
- Run A/B tests on cadence/content and affordability support;
- Scale what lifts adherence and experience.
How Pulse helps: Out-of-the-box dashboards and cohort diffs to show lift early and often.
Risks & pitfalls to avoid
- Treating “patient-centric” as a campaign — not an operating model.
- Over-personalization without explicit consent and clear expectations.
- Accessibility as an afterthought (retrofits cost more and miss people).
- Weak change control around content that requires MLR.

How Pulse helps: Consent scopes/frequency guardrails; WCAG checks; change-management and release controls.
Get Started with Pulse Health Today
Patient-centricity is where policy momentum, interoperable data, and experience measurement meet. You don’t need a full replatform to see impact — launch a focused 90-day pilot, prove lift on time-to-therapy and persistence, then scale confidently.

See how Pulse operationalizes patient-centric marketing — book a 30-minute blueprint session.
Frequently Asked Questions
Designing end-to-end journeys around patient needs, constraints, and preferences — using consented data, accessible content, and outcome-based KPIs — to improve access, adherence, and patient-reported outcomes (PROs). See FDA’s Patient-Focused Drug Development.
A PSP (benefits checks, copay/PAP, nurse support) is one component. Patient-centric marketing is the operating model that unifies PSPs with omnichannel education, accessibility (WCAG 2.2), data governance, and outcomes measurement across the lifecycle.
Track time-to-therapy, first-fill, 90-day persistence, PRO deltas, and experience metrics aligned with CAHPS. Tie changes to specific journey interventions (e.g., affordability prompts, refill nudges) for clear attribution.
Yes — when consent capture, BAAs, role-based access, and audit trails are embedded, and electronic records/signatures align to HIPAA Rules and 21 CFR Part 11.
Run a 12-week pilot: select one condition and two personas, deploy a consented WCAG-aligned journey (SMS/email/portal + human handoffs), benchmark KPIs, and A/B test cadence, language, and affordability support. Scale what moves time-to-therapy and persistence.
HL7 FHIR and national exchange under TEFCA reduce data friction between hubs, PBMs, and providers — enabling timely outreach (e.g., prior-auth status or refill gaps) without copy-pasting data.
They close the loop between education/support and outcomes. FDA’s programs around RWE and guidance on PROs help teams justify investments and refine journeys.
Build to WCAG 2.2 (alt text, captions, keyboard navigation, readable typography, low-bandwidth options) and align language/culture with the National CLAS Standards.
Use translation memory, interpreter routing, and culturally appropriate copy guided by CLAS. Validate with native-speaker review and usability tests for key flows (onboarding, PA, refills).
Via REST APIs, webhooks, and standards-based connectors (FHIR/HL7). We can ingest from EHRs/hubs/PBMs and push updates to your CRM or data warehouse; details depend on your architecture — reach out and we’ll map an integration brief.