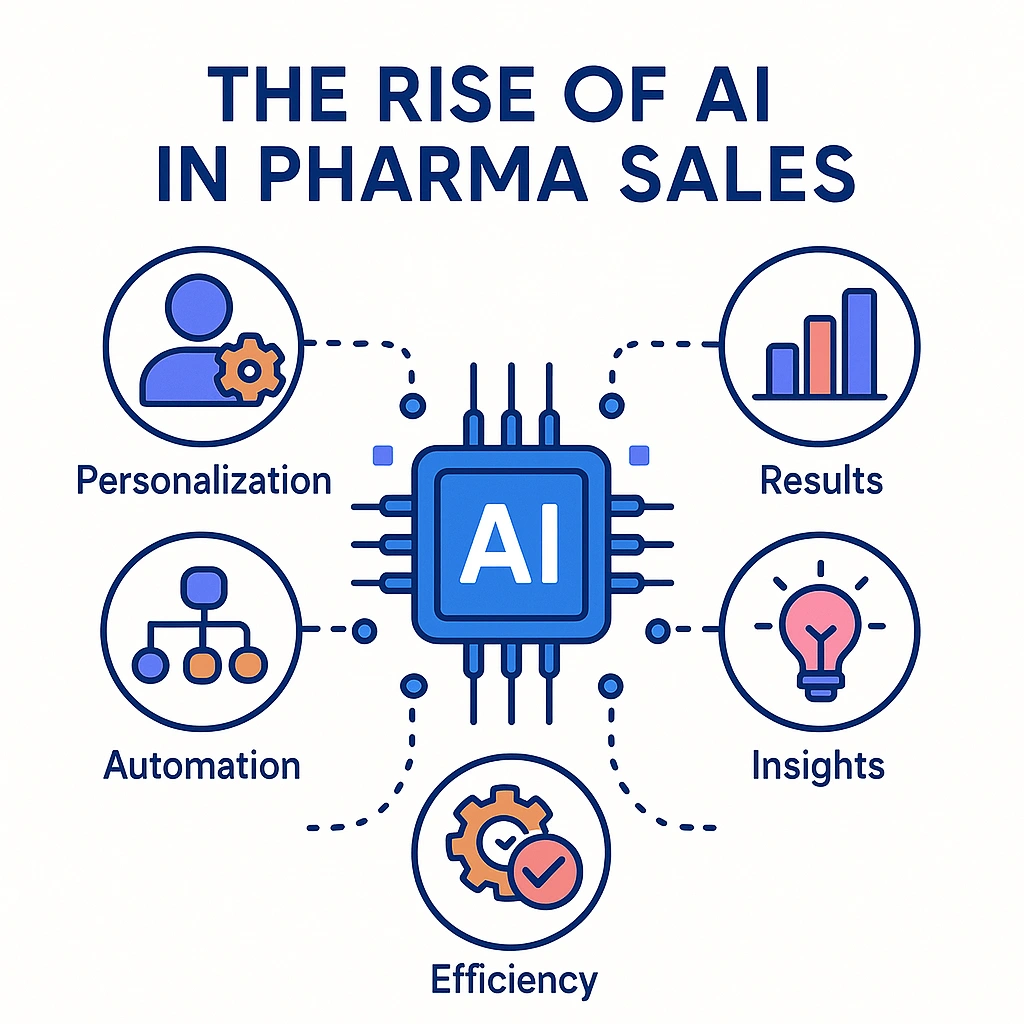
The Rise of AI in Pharma Sales
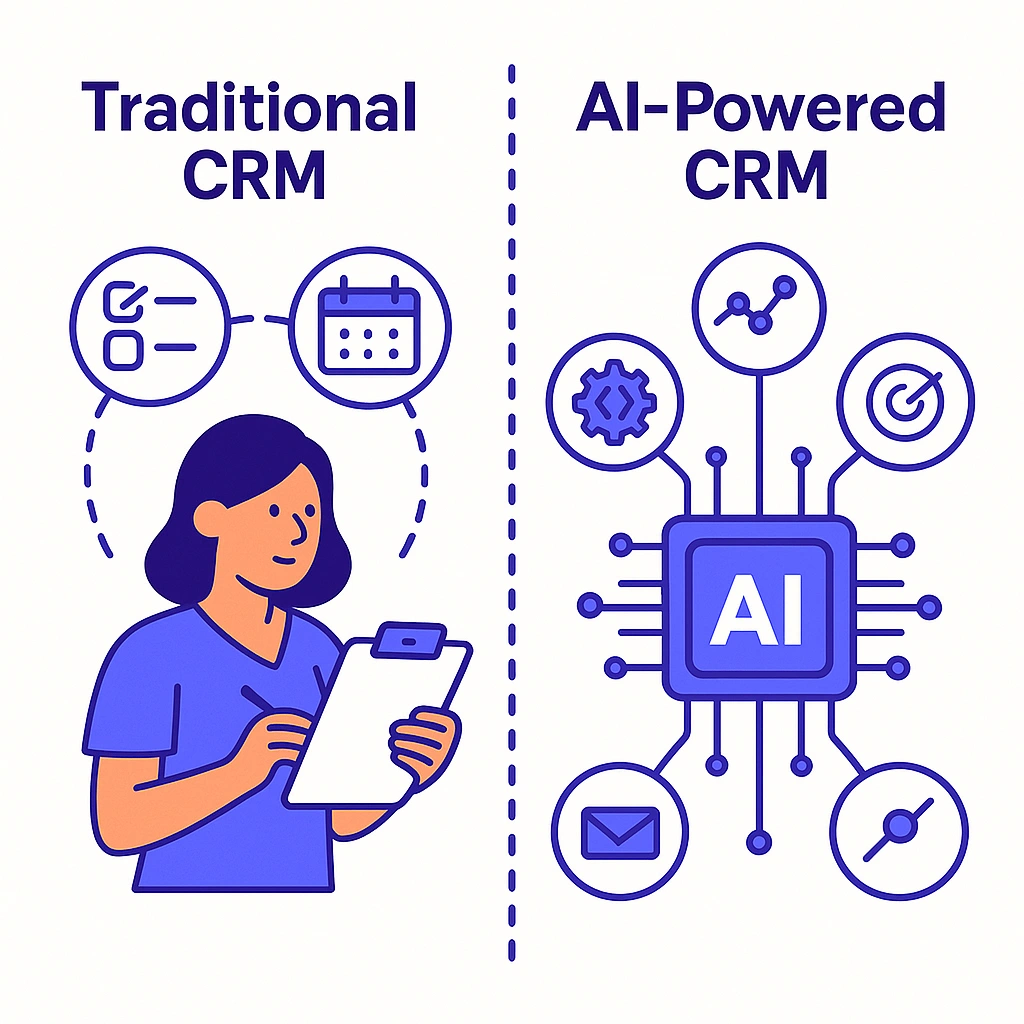
Pharma sales has never had more data — or higher stakes. Traditional CRMs help teams log calls and track accounts, but they rarely answer the questions that change outcomes: Which HCP should I speak with today? What should I send? How do I follow up compliantly — and fast?
AI-powered CRMs close that gap by turning scattered sources (claims, formulary, CLM, hub, consent, and field notes) into precise next-best actions, compliant content suggestions, and time-saving copilot workflows.
The result is more high-quality HCP engagements, better territory execution, and measurable commercial impact without adding admin burden.
With the right data foundation, governance, and change-management plan, teams can pilot within a quarter and scale across brands. This article explains how — step by step — and where Pulse Health fits.
The State of Pharma Sales & Why Traditional CRMs Stall
A conventional CRM is a system of record. That’s essential, but not sufficient. In most organizations, core information sits in silos: CRM activities, CLM/eDetail analytics, formulary/access changes, specialty pharmacy and hub status, conference interactions, consent and channel preferences, and third-party claims data. Reps and MSLs spend valuable time digging for signals, reconciling conflicting sources, and writing notes that are more about compliance than coaching the next move.
At the same time, customer expectations have shifted:
HCPs expect precision: fewer, more relevant touches and content that respects their specialty, patient population, and schedule. Brand and
Compliance teams expect rigor: claims bound to labeling, traceable sources, and standard operating procedures for adverse event capture.
Field managers expect visibility: whether activities translate into higher-quality meetings, better pull-through following access updates, and steady NBRx/TRx progress across targets.
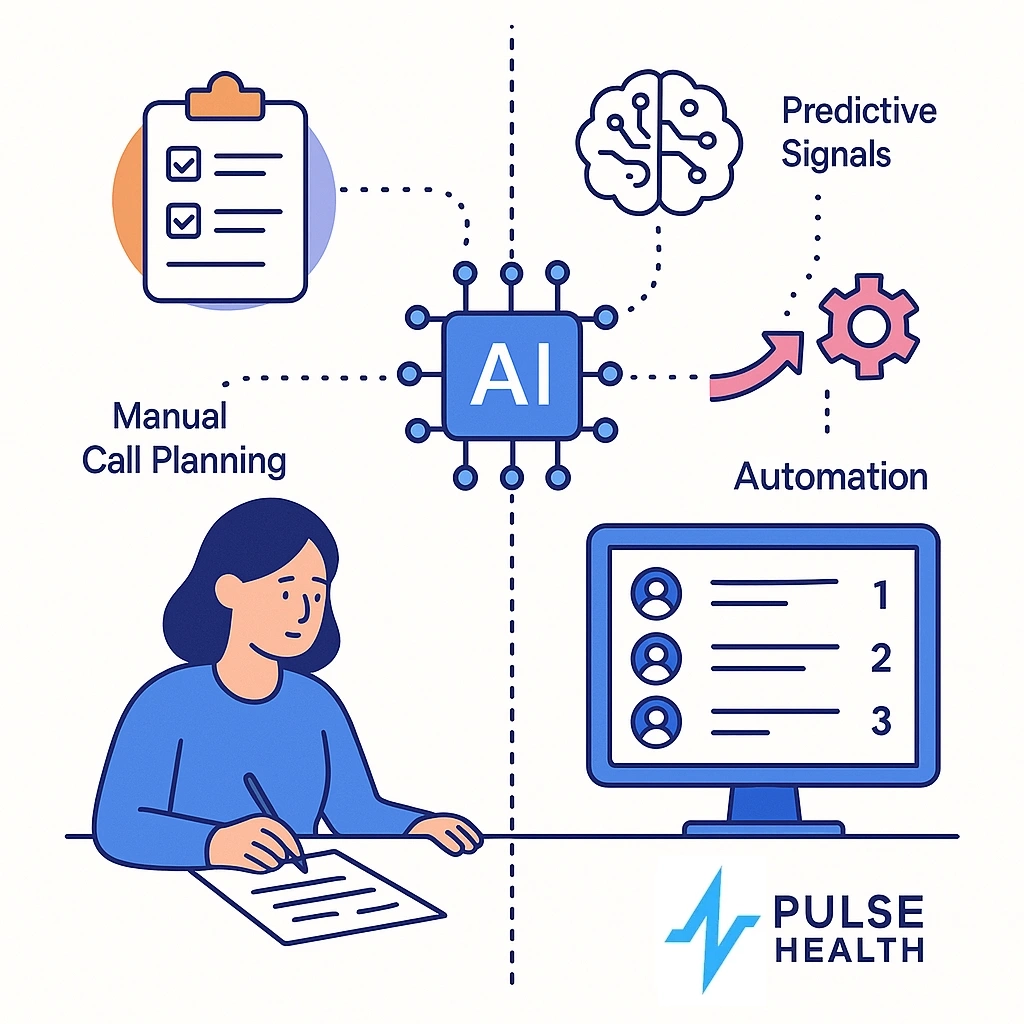
Traditional CRMs don’t fail because they’re missing fields; they fail because they lack judgment. They’re built to store what happened, not to suggest what should happen next. AI-powered CRMs add that missing layer of prioritization, context, and automation — within MLR guardrails — so the system of record becomes a system of action.
Old vs. New
| Capability | Traditional CRM | AI-Powered CRM |
| Call planning | Static target lists; manual filtering | Daily ranked HCP list with “why now” reasons tied to signals |
| Personalization | Generic templates | Compliant content recommendations by persona, lifecycle stage, and recent behavior |
| Objection handling | Search PDFs during/after call | On-call retrieval from approved sources with labeled citations |
| Forecasting | Top-down targets | Bottom-up forecasts from activity quality + cohort signals |
| Compliance logging | Manual notes | Auto-summaries with AE detection, citations, audit trails |
What to do next: Write down the three questions you wish your CRM answered every morning. If they include “who, what, and why,” you’re ready for AI.

What We Mean by an AI-Powered CRM in Pharma
“AI-powered” isn’t a separate dashboard or a new analytics portal. It’s intelligence embedded where people work: in the call plan, the email composer, the meeting summary, the coaching dashboard. It blends two complementary capabilities:
- Predictive AI that scores targets, surfaces signals, and prioritizes next-best actions (NBA) across channels.
- Generative AI that drafts compliant emails, summarizes calls, and retrieves labeled responses — constrained by approved claims and medical content.

Crucially, this isn’t a black box. AI recommendations carry transparent reasons (e.g., “Formulary update for Plan X; Dr. Lee’s last CLM showed interest in adherence content; 30-day gap since last high-quality interaction”). Human reviewers can accept, modify, or dismiss each suggestion. Governance is built in: approved content libraries, prompt templates aligned with labeling, automated citations, role-based access, and full audit trails.
What to do next: Identify where reps spend >20 minutes/day on low-value admin. Those are your first copilot use cases.
Getting the Data Foundation Right
You don’t need a “perfect” warehouse to start, but you do need a trustworthy one. Focus on five foundations:
1. Sources that matter most
- CRM: Accounts, contacts, calls, events, tasks, samples.
- CLM/eDetail: Asset IDs, dwell time, completion, page-level interactions.
- Access & coverage: Formulary status, PA requirements, tier changes.
- Hub/specialty pharmacy (where applicable): Enrollment, PA initiated/approved, first fill, specialty rejections (governed for patient privacy)
- Claims & affiliations: Targeting cohorts, decile movements, group practices, IDN structures.
- Consent & preferences: Channel permissions, quiet hours, opt-ins.
- Conferences & KOL interactions: Sessions, posters, touchpoints.
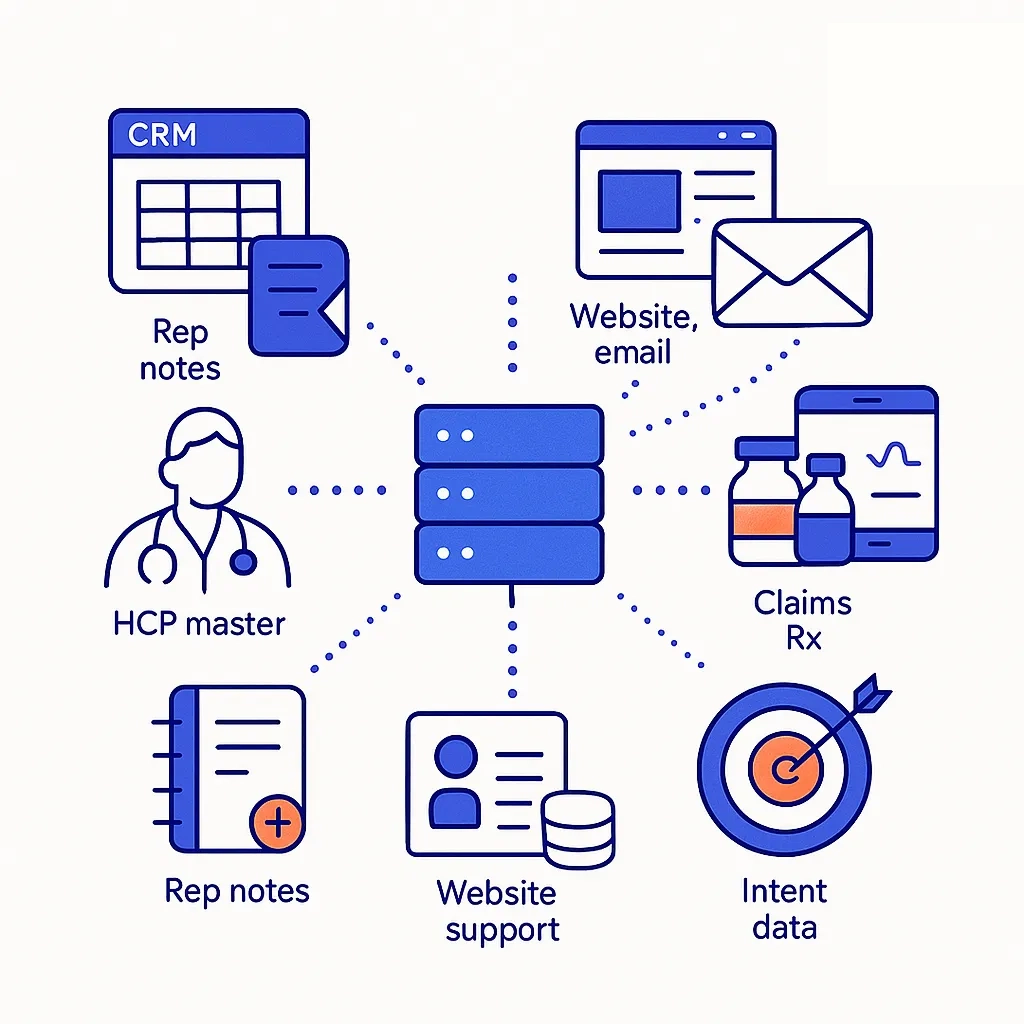
2. Identity resolution

Unify HCP/HCO records, NPI/DEA identifiers, affiliations, and care team links.
Poor identity mapping is the #1 source of noisy recommendations.
3. Freshness & quality SLAs
Decide how often each source updates (daily/weekly), define validation checks, and trace lineage so analysts can explain why an HCP appears in the call plan.

4. Consent-aware orchestration
AI must respect channel permissions by design: email/SMS/remote visit sequencing should only trigger within documented consent.
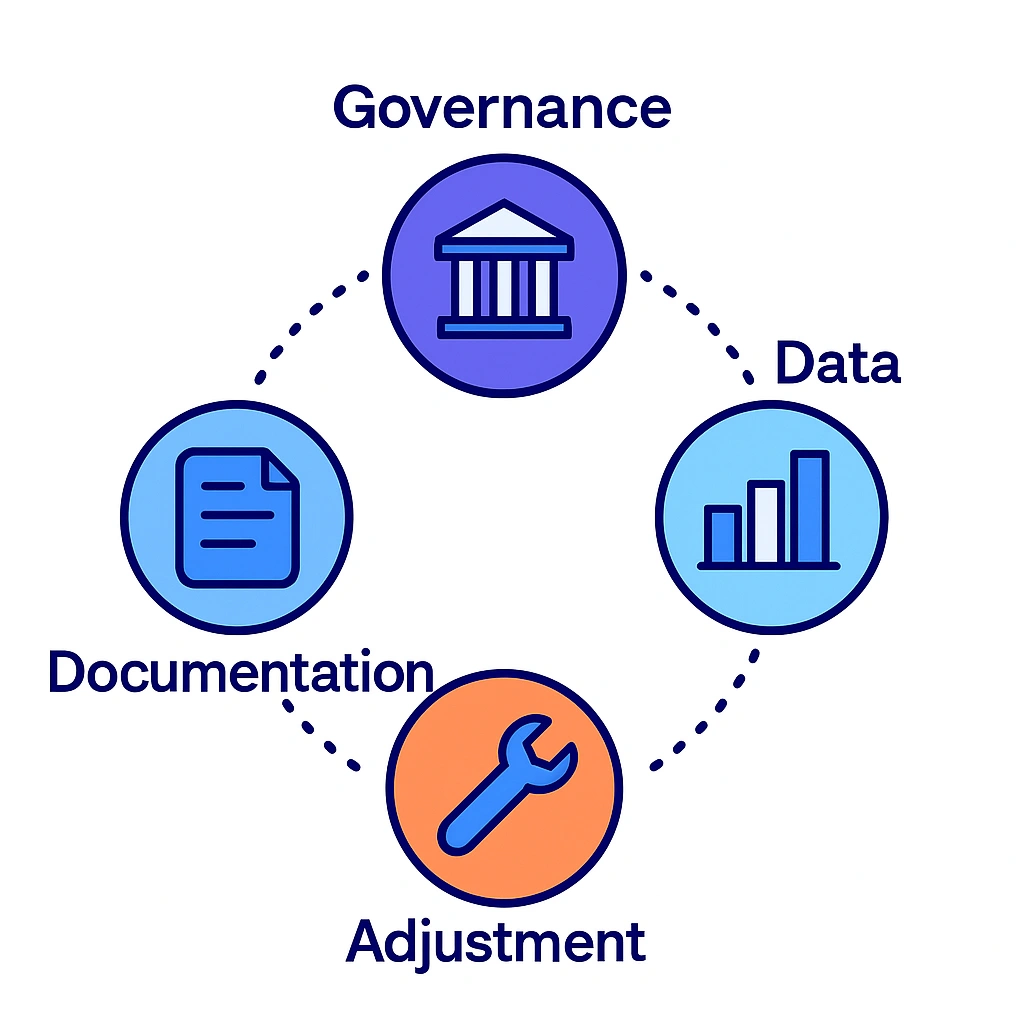
5. Audit-ready governance
Keep versioned models, prompts, content libraries, and output logs.
Capture adverse events (AEs) and route them to the right teams.

Minimum viable data to start: CRM + CLM + access/coverage + consent.
Nice-to-have enrichments: Claims cohorts, hub status signals, conference/KOL graphs, longitudinal adherence proxies.
What to do next: Build a one-page “data contract” stating sources, update cadence, and data owners. It’s the fastest path to alignment with Medical/Legal/Regulatory (MLR) and IT.
AI Capabilities That Actually Move the Needle
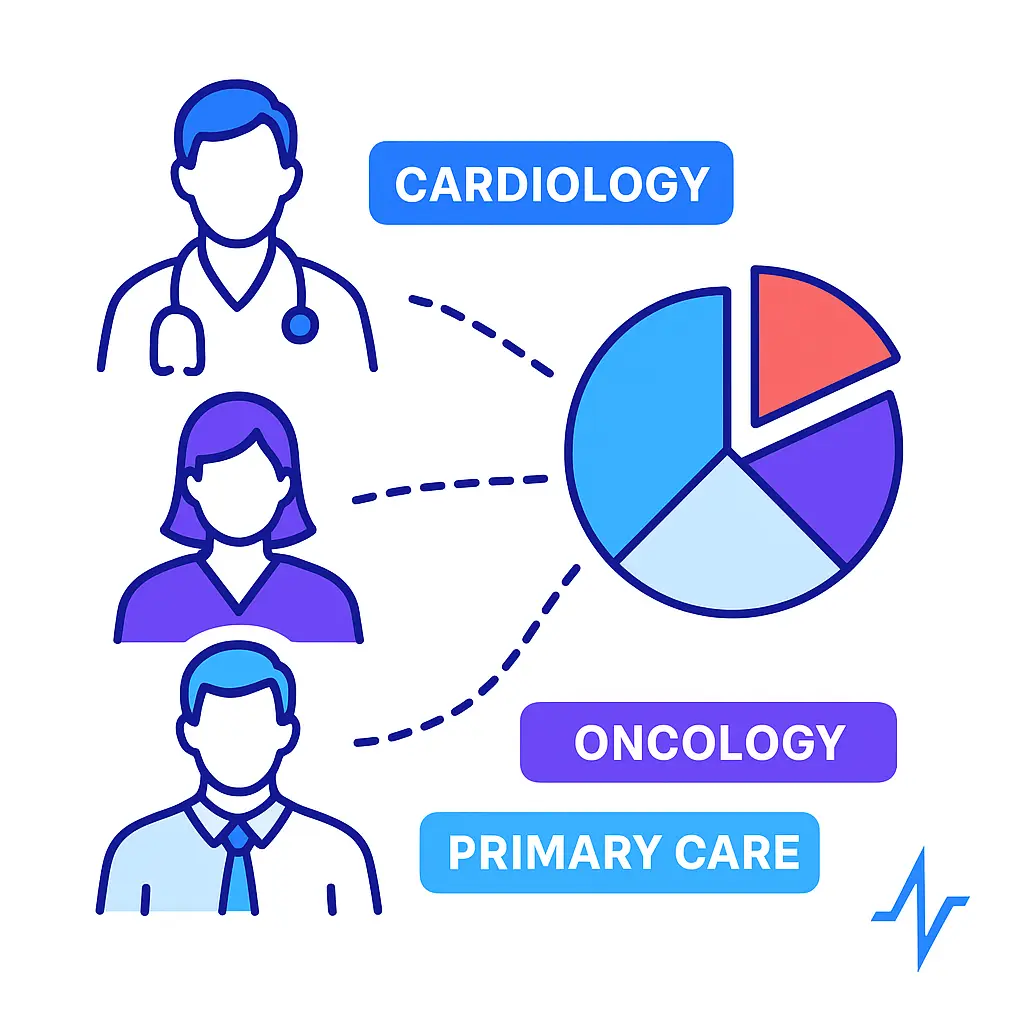
Predictive Targeting & Lead Scoring
What it does: Surfaces HCPs with rising relevance — e.g., coverage wins in their dominant plan, growing patient cohorts, or recent engagement with disease-education content.
How it works: Models weigh signals such as last high-quality interaction, formulary shifts, content resonance by specialty, and geographic pull-through patterns.
The output is an ordered list for each territory with “reason codes” so reps understand why an HCP is prioritized.
Track it with: Meeting-set rate for priority HCPs, ratio of high-quality to low-quality calls, incremental NBRx in the focus cohort (directionally, without over-attribution).
Before/after: Instead of mass filtering a static target list every Monday, reps start each day with a list that already knows what changed since yesterday.
Next-Best-Action (NBA) & Call Planning
What it does: Converts scores and signals into a daily plan: who to see, which channel to use, what content to lead with, and suggested follow-up.
How it works: NBA considers consent, channel preferences, recency/frequency, access events, and CLM performance to sequence outreach.
It explains “why this HCP, why today,” and enforces quiet hours or MLR constraints on messages.

Track it with: Reduction in low-value touches, increased reach among high-potential HCPs, on-time follow-ups after access events.
Before/after: “I guess I’ll call on everyone in my A-list” becomes “These five HCPs today, email these three, and hold content X for Dr. Shah because of yesterday’s plan change.”
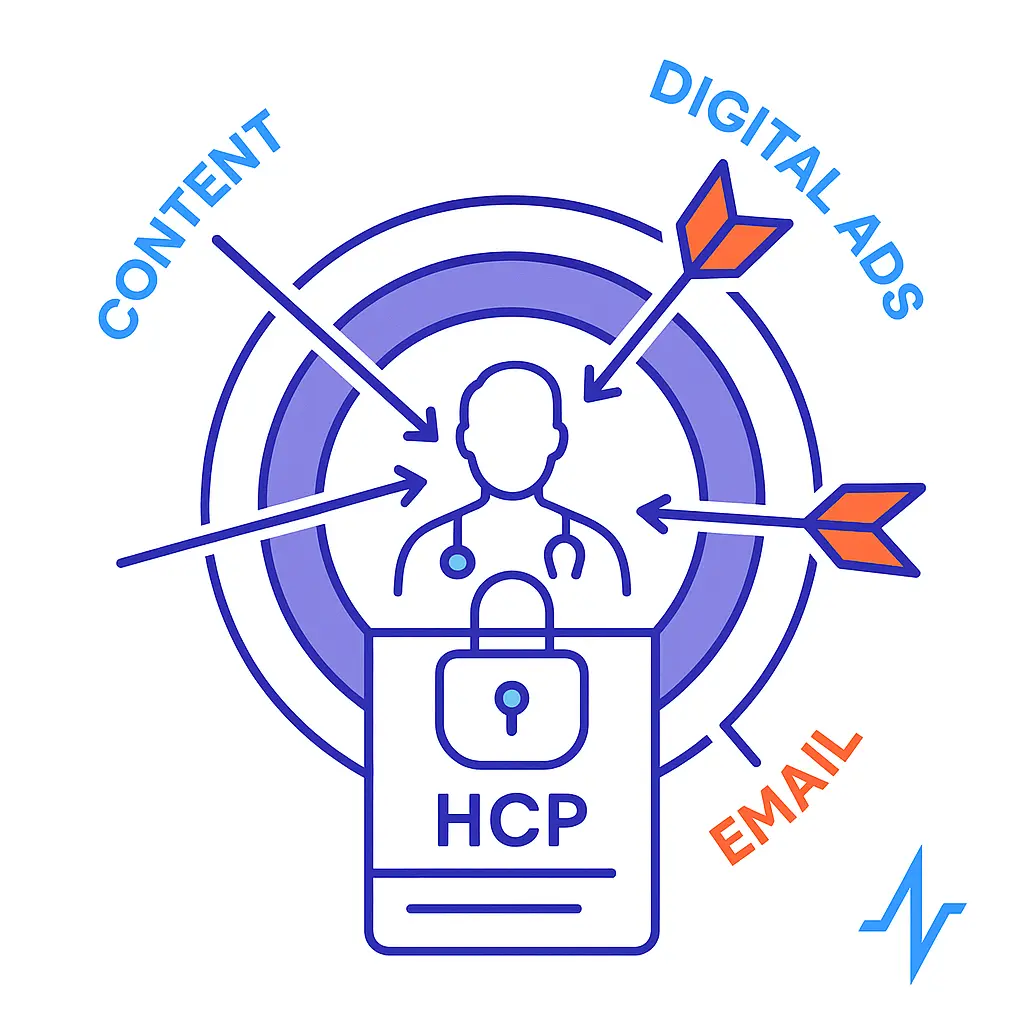
Personalization at Scale (MLR-Safe)
What it does: Recommends approved content that matches the HCP persona and moment — without wandering beyond label.

How it works: CLM analytics feed a recommender that ranks assets for each audience and situation (e.g., early adoption vs. cost concerns).
Generative AI assembles the email opening and call outline but only with approved claims, references, and tone.
Track it with: CLM completion rate and dwell time on priority assets, replies/meeting bookings from compliant emails, downstream requests for medical information.
Before/after: Templates no one reads become targeted touchpoints with a clear educational purpose.
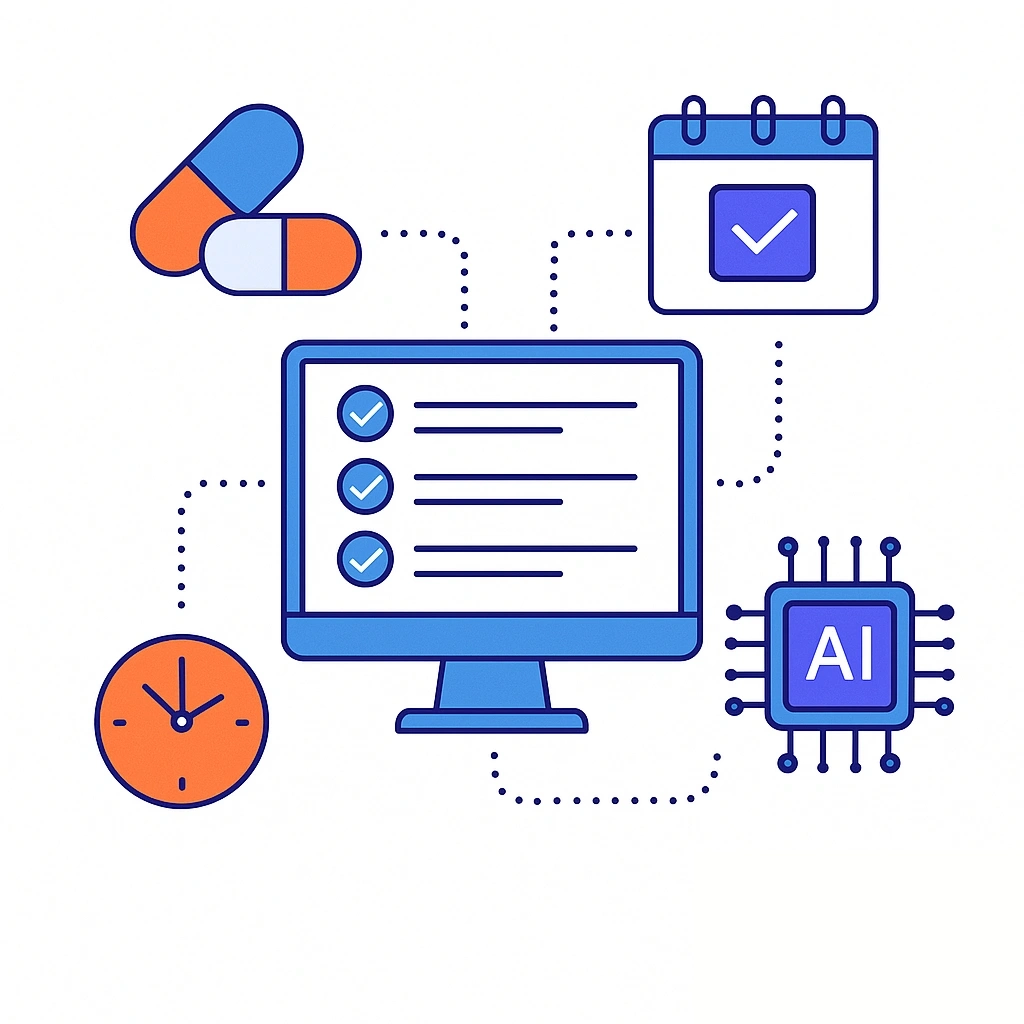
Rep Copilot for Admin Reduction
What it does: Transcribes visits, summarizes key points, flags potential AEs, and drafts structured follow-ups — ready for human review.
How it works: Voice or typed notes run through domain-tuned models with AE detectors and citation engines.
Summaries post to the CRM with standardized fields so managers can coach to quality, not just quantity.
Track it with: Minutes saved per call report, speed-to-follow-up, completeness of mandatory fields (without adding clicks).
Before/after: Thirty minutes of “after-call admin” becomes five minutes of review and refinement.
Real-Time Objection Handling & Knowledge Retrieval
What it does: Brings the right, approved information to the rep during conversations.
How it works: Retrieval-augmented generation (RAG) constrained to PI, FAQs, and MLR-approved materials returns an answer with inline citations.
If content isn’t approved for promotional use, the copilot routes to Medical with the proper workflow.
Track it with: Objection resolution rate, time to escalate to Medical when appropriate, accuracy and citation compliance scores.
Before/after: Tab-hunting through PDFs becomes “Here’s the response with a citation to Section 5.2 of the PI.”
Territory & Route Optimization (Field & Inside)
What it does: Optimizes the mix of in-person vs. remote touches and clusters visits to cut travel time while protecting HCP preferences.
How it works: NBA overlays geography and calendar, groups nearby high-priority HCPs, and recommends virtual follow-ups where in-person adds limited incremental value.

Track it with: Visits per day, travel time reduction, adherence to channel preferences.
Before/after: “I’ll drive the usual loop” becomes “Two micro-clusters near the hospital today plus three remote follow-ups.”
Forecasting & Pipeline Health
What it does: Produces bottom-up forecasts tied to activity quality and cohort signals rather than pure volume.
How it works: Models link leading indicators (content engagement, meeting quality, access changes) to downstream script patterns.
Managers see variance explanations instead of just variance.
Track it with: Forecast accuracy, percentage of variance with clear reasons, earlier detection of soft spots.
Before/after: Retroactive adjustments become proactive course-corrections.
Signal Capture from Patient Support/Hubs (Where Applicable)
What it does: Uses governed, de-identified signals (e.g., PA milestones, first-fill status) to trigger timely pull-through education for HCP offices.
How it works: When a patient reaches a new step (PA initiated/approved), NBA suggests a compliant office follow-up (e.g., benefits verification refresher), respecting privacy and role boundaries.
Track it with: Time-to-therapy, first-fill rate proxies, decrease in preventable abandonment signals.
Before/after: One-off office check-ins become precise, helpful timing aligned to actual patient journeys — ethically and compliantly.
What to do next: Pick two capabilities for a pilot: one that saves time (copilot) and one that improves quality (NBA/personalization).
Role-Based Use Cases
Field Sales Reps

Start the day with an ordered call plan, a short rationale per HCP, and two suggested assets.
After each interaction, the copilot drafts a summary, highlights next steps, and prepares a compliant email with citations.
Reps spend more minutes with HCPs and fewer minutes with forms.
Micro-playbook: Following an access update, send an approved coverage overview, schedule a brief office in-service, and log any office barriers. The copilot builds the sequence and reminders.
Key Account Managers (KAM)
For IDNs and large groups, KAMs need a 360° view: decision makers, care pathways, P&T timelines, and clinics showing rising patient cohorts.
AI reveals stakeholders to sequence, maps influence across departments, and proposes coordinated touches that don’t overwhelm the account.
Medical Science Liaisons (MSLs)
MSLs require precision and separation from promotion.
AI maintains literature watchlists, tracks scientific engagement history, and visualizes KOL networks.
The copilot helps compile compliant scientific summaries and field insights for Medical — not for promotion — ensuring governance lines are respected.
Inside Sales / Remote Engagement
Sequenced outreach mixes email, remote visits, and portal messaging based on consent and preference.
The system paces contact to avoid fatigue, suggests educational content matched to recent questions, and alerts reps to “best window” times for specific HCPs.
Brand & Field Excellence

AI closes the loop between content and outcomes. CLM analytics and rep feedback feed creative briefs: which messages resonate, which objections persist, which visuals drive completion.
Brand teams prioritize updates where they will matter most.
Access/Payer Teams (as appropriate)
When coverage shifts, AI coordinates pull-through across roles.
KAMs and reps receive “reason codes” tied to affected HCP panels, suggested touch patterns, and office resources to reduce administrative friction.

What to do next: Define two role-specific success metrics (e.g., time-to-follow-up for reps; completion of cross-stakeholder sequences for KAMs) to evaluate any pilot.
Compliance, Privacy, and Model Governance
AI only works in pharma when governance is first-class. Build your controls in layers:
- Regulatory scope: HIPAA (where applicable), 21 CFR Part 11 for electronic records and signatures, GDPR/CCPA and state privacy laws, Sunshine Act and aggregate spend, PDMA/sample tracking, AE reporting workflows.
- Guardrails by design:
- Approved claims libraries and PI documents are the only sources the copilot may cite for promotional use.
- Prompt templates are version-controlled and reviewed by MLR.
- Red-flag terms trigger Medical escalation rather than promotional reply.
- Human oversight: Every AI output is editable; reviewers can accept, modify, or reject with feedback that trains future suggestions.
- Traceability: Store model versions, prompts, inputs, and outputs with timestamps and user IDs. Maintain retention schedules and access logs.
- Model risk management: Monitor drift, measure false-positive/false-negative rates for AE detection, and run periodic fairness/variance checks.
- Separation of duties: Ensure Medical, Commercial, and Compliance use the same knowledge base under different policies and interfaces.
What to do next: Run a half-day governance workshop to agree on “approved corpora,” escalation paths, and release criteria before writing a single line of production prompt code.
Integrations & Architecture for Pharma Stacks
An AI-powered CRM succeeds when it fits into the ecosystem you already use:

- Core CRM/CLM: Bi-directional sync with leading platforms (accounts, activities, CLM asset IDs, content engagement).
- Data & identity: Secure connectors to claims/affiliation providers, access/coverage feeds, and identity graphs; deterministic + probabilistic matching.
- Consent & outreach: Integration with consent systems and channel tools to enforce permissions in real time.
- Voice & notes: Call recording/transcription with domain vocabularies; PII scrubbing where appropriate.
- Security & IT controls: SSO, SCIM provisioning, role-based access, bring-your-own-key (BYOK) options, network allowlists, and offline-capable mobile.
Architecture principle: Orchestrate, don’t replace. Your CRM remains the source of record; Pulse Health provides the reasoning layer (NBA, copilot, governance) that sits in front of it.
What to do next: Map one territory’s data flows end-to-end. If an analyst can trace “this email draft cites that PI paragraph,” you’re integration-ready.
Measuring Impact & Building the Business Case
North-star outcomes (directional):
- Higher-quality HCP engagements and meeting-set rates among priority segments
- Faster, more consistent follow-ups after access changes
- Steadier NBRx/TRx growth within targeted cohorts

Leading indicators (what you’ll see first):

- Increased CLM completion and dwell time for priority assets
- Reduced time-to-follow-up and more complete call records
- Higher reply rates to compliant emails; more scheduled remote visits
Experiment design:
- Start with A/B territories or staggered rollouts; track pre/post baselines
- Use matched cohorts to reduce bias
- Tie each capability to 1–2 metrics you can measure weekly

ROI framing:

- Time saved × rep/manager cost (hard dollars)
- Incremental scripts × margin assumptions (directional value)
- Risk reduction from standardized, traceable communications (qualitative but meaningful)
Metrics hierarchy (example)
| Layer | Example Metrics |
| Activity | Calls, emails, remote visits, CLM views |
| Quality | Meeting length, CLM completion, objection resolution |
| Outcome | Meeting-set rate, time-to-therapy proxy, pull-through after access events |
| Financial | Incremental NBRx/TRx trends in targeted segments |
What to do next: Choose one capability that shows impact in <60 days (e.g., copilot summaries) and one that compounds over a quarter (e.g., NBA). Define baseline and acceptance criteria now.
Implementation Roadmap: From Pilot to Scale
Phase 1 — Discovery & Success Plan (2–3 weeks)
Clarify use cases, KPIs, territories, and data owners.
Align with MLR on approved corpora and review workflows. Document acceptance criteria.

Phase 2 — Data & Governance Readiness (2–4 weeks)
Wire core sources (CRM, CLM, access, consent).
Validate identity resolution.
Stand up audit logging and role-based controls.
Finalize AE routing.
Phase 3 — Content & MLR Alignment (in parallel)
Assemble approved claims, PI, FAQs, and email templates.
Version prompts.
Agree on red-flag lists and Medical escalation paths.
Phase 4 — Pilot (8–12 weeks)

Limit scope (one brand/region).
Train champions.
Run weekly QA on outputs.
Iterate on reason codes and content recommendations.
Track leading indicators weekly.
Phase 5 — Scale & Change Management (6–10 weeks)
Codify playbooks, office hours, and manager coaching.
Expand to additional regions/brands. Automate more of the data quality checks.

Phase 6 — Continuous Optimization (ongoing)

Quarterly model refreshes, prompt tuning, and content updates.
Add new signals (e.g., conference engagements), retire noisy ones.
Review governance logs.
What to do next: Appoint a cross-functional “AI CRM Tiger Team” (Sales Ops, Brand, IT, MLR, Field) with a weekly stand-up and a single shared scorecard.
Case Snapshots (Anonymized)
Specialty Launch Team (U.S.)
Situation: New therapy with complex access; 65 reps across 8 regions.
Action: Rolled out NBA for coverage-triggered outreach and copilot summaries.
Result: Reps reported fewer missed follow-ups after plan changes and faster, more consistent compliant emails.
Managers saw steadier meeting-set rates in priority HCPs.
Primary Care Brand (EU)
Situation: Large target list; message fatigue risk.
Action: Consent-aware sequencing with content recommendations per persona.
Result: Higher CLM completion on core assets and improved reply rates to remote-visit invites, especially among previously low-engagement segments.
Rare Disease Team (U.S.)
Situation: Small HCP universe; scientific depth critical; Medical/Commercial separation paramount.
Action: Medical used a non-promotional copilot to compile literature digests and KOL interaction summaries; reps used NBA for timing and channel mix only.
Result: Better coordination without promotional spillover; faster literature responses for HCP scientific queries.

Buyer’s Checklist: Questions to Ask Vendors

Data & Identity
- Which sources do you natively connect to? How do you handle identity resolution across HCP/HCO/IDN? What are your data freshness SLAs?
Governance & MLR
- Show your prompt/version control and audit logs. How are AE detections routed? Can we restrict corpora to approved content only?
NBA Transparency
- Do recommendations include reason codes? Can field managers see the feature importance behind prioritization?
Content/CLM Fit
- How do you map CLM assets to personas and lifecycle stages? Can we test variants within approved claims?
Mobility & UX
- Offline support? One-tap accept/edit for copilot drafts? Admin clicks saved per call report?
Security
- SSO/SCIM, BYOK, network controls, regional data residency.
Services & Change Management
- Field training, playbooks, office hours. How do you partner with Medical and Compliance during rollout?
Pricing & Value
- Clear unit of value (per user, per brand). How do you model ROI and what metrics do you instrument out of the box?
Common Pitfalls & How to Avoid Them

- Over-personalization without guardrails: Enforce labeling via approved corpora and standardized prompts.
- Black-box recommendations: Require reason codes and explainability.
- Click-heavy workflows: Design for two clicks or fewer to accept/edit AI outputs.
- Messy identity data: Invest early in HCP/HCO resolution; it multiplies downstream quality.
- Vague pilots: Define acceptance criteria and a fixed timeline; celebrate wins and kill what doesn’t work.
- No Medical partnership: Bring Medical in from day one; separate promotional and scientific use cases.

What’s Next: Emerging Trends

- Real-time access signals: Closer coordination with hubs and payers (governed and consent-aware) to time education around actual administrative milestones.
- Multimodal copilots: Voice + screen experiences that draft summaries and surface citations mid-visit with minimal cognitive load.
- Dynamic CLM sequencing: Auto-assembled flows from approved micro-assets tailored to persona and meeting stage.
- Shared knowledge bases: Medical and Commercial access the same source of truth with role-appropriate guardrails, reducing inconsistent messaging.
How Pulse Health Helps
Pulse Health turns your CRM into a daily advantage by combining transparent NBA, a compliant copilot, and governance you can trust.
- Pulse NBA Engine
Produces ranked daily call plans with clear reason codes (“Why this HCP now”) drawn from access updates, CLM performance, consent, and recent interactions. Managers see territory-level patterns and can coach to quality, not just counts. - Compliant Copilot
Drafts follow-up emails and visit summaries using only approved claims and PI sources, with inline citations and AE detection. Every output is editable; accept or modify in seconds. - CLM Optimizer
Recommends the next approved asset per persona and lifecycle stage, turning content analytics into action.

- Voice-to-Notes
Accurate transcription tuned for medical vocabulary, plus structured summaries that populate CRM fields consistently. - Access Signals Connector
Surfaces formulary and benefit changes in context so reps can time education and office support more effectively — within consent and privacy constraints. - Governance Hub
Versioned prompts, content libraries, and model artifacts with role-based access, audit logs, and robust AE routing — built for MLR collaboration.
Why teams choose Pulse Health: measurable time savings, higher-quality interactions, and a rollout approach that brings Medical, Compliance, and IT along from the start.
Get Started with Pulse Health Today
AI inside the CRM isn’t about more dashboards. It’s about waking up to a plan you trust, conducting fewer but better conversations, and following up with compliant precision — without spending your evening on admin. With a pragmatic data foundation, clear governance, and a right-sized pilot, pharma sales teams can turn intelligence into outcomes in a single quarter and scale from there.
Ready to see it in action?
Schedule a Pulse Health demo and we’ll map the first 90-day plan for your brand and territory.

Glossary of Key Terms
AE (Adverse Event): Any untoward medical occurrence associated with a product. Must be captured and routed per policy.
CLM (Closed-Loop Marketing): Digital detailing where content engagement feeds back into planning.
IDN (Integrated Delivery Network): Health system coordinating care across facilities.
KAM (Key Account Manager): Role focused on multi-stakeholder accounts (e.g., IDNs).
KOL (Key Opinion Leader): Influential clinician or researcher within a field.
MLR (Medical-Legal-Regulatory): Cross-functional review that approves content and processes.
NBA (Next-Best-Action): Prioritized recommendation of who/what/when/why for outreach.
NBRx/TRx: New-to-brand prescriptions / total prescriptions.
PI (Prescribing Information): Labeling content approved for promotional use.
RAG (Retrieval-Augmented Generation): Technique where generative models retrieve approved documents to ground answers.
Frequently Asked Questions
Dashboards describe the past. AI-powered CRM recommends the next action — who to contact, which channel, and what to send — with transparent reasons and one-click execution.
Best practice is human-in-the-loop: use approved templates and claims libraries so drafts are close to ready, then have users or reviewers approve before sending per your MLR policy.
Begin with CRM, CLM analytics, access/coverage feeds, and consent. Add claims cohorts, hub signals, and conference/KOL data as you mature.
Use governed, consent-compliant signals. Restrict promotional copilots to approved corpora, scrub PII where required, and route AEs appropriately.
Each recommendation includes reason codes and link-outs to the signals used. Managers see feature importance and can give feedback that tunes future suggestions.
Many teams pilot in 8–12 weeks after alignment on data and governance. The key is scoping: one brand/region, two or three high-impact use cases, clear acceptance criteria.
Yes, but with different emphasis. NBA leans more on consented preferences and scientific interest signals; Medical and Commercial separation is paramount.
Short, scenario-based sessions (90–120 minutes) plus office hours. Focus on accepting/editing suggestions, using citations, and giving feedback.
Copilot detectors flag potential AEs in notes and emails, pause promotional sends, and route to the approved pharmacovigilance workflow with an audit trail.
Start with a cleaning sprint: unify HCP/HCO IDs and affiliations. Identity resolution quality is the single strongest predictor of NBA usefulness.