A practical guide for pharma manufacturers in the U.S. and Canada
Pharma engagement lives under some of the strictest rules anywhere. Every email to an HCP, SMS to a patient, or sample drop has regulatory fingerprints — from the U.S. FDA Office of Prescription Drug Promotion (OPDP) and Prescription Drug Marketing Act (PDMA), to HIPAA’s Privacy Rule, to CMS Open Payments, to Canada’s PAAB pre-clearance code, Health Canada advertising guidance, CASL anti-spam, and PIPEDA. The goal of this guide is simple: show you how to embed these guardrails into everyday work — so compliance becomes the engine of trust, not a brake on go-to-market velocity.

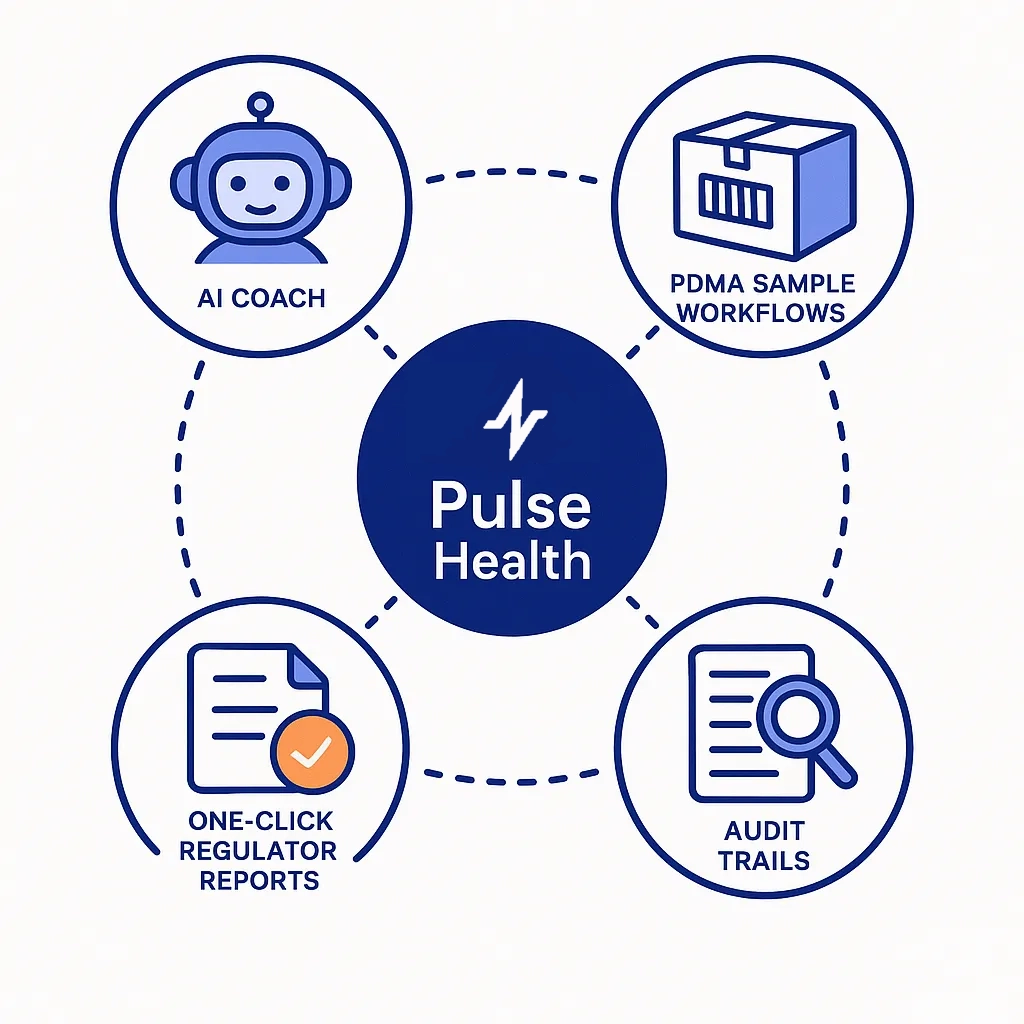
Throughout the article, we’ll also flag where Pulse Health can take heavy lifting off your team — omnichannel logging, consent capture, AI compliance monitoring, PDMA-safe sample workflows, one-click regulator reports, and deep integrations with field tools like Veeva and message partners like OptimizeRx.
The Rules That Shape Your Communications
Before we talk tactics, it’s worth grounding the conversation in the rules that actually shape what’s possible. The guardrails aren’t abstract — they dictate how you write an email, what a rep can say on a call, and even how a sample changes hands.
Here’s what pharma regulators care about (in plain English):
Truthful, non-misleading promotion (on-label only):
OPDP expects fair balance and adequate risk disclosure in all promotional labeling and advertising (FDA OPDP).


Adverse events must be captured and reported quickly:
Serious/unexpected events often follow tight windows (e.g., IND safety reporting under the FDA’s IND reporting framework).
Patient privacy and consent:
Handle PHI per the HIPAA Privacy Rule; if you operate globally, align with GDPR principles too.

HCP transfer-of-value transparency (U.S.):
Track, aggregate, and report per the Sunshine Act / Open Payments.
Samples are tightly controlled:
Document prescriber requests, receipts, inventory, and limits under PDMA.

Anti-spam & consent for digital marketing:
U.S. CAN-SPAM (FTC overview) and TCPA (FCC TCPA) govern email and phone/SMS; Canada’s CASL requires express opt-in and documented consent flows.
Canada’s content posture:
DTC prescription promotion is heavily restricted; HCP-facing materials often need PAAB pre-clearance and must align to Health Canada guidance.
Canada vs. U.S.: What Changes for Pharma CRM & Communications
Most of this article centers on U.S. rules. If you operate in Canada too, a few structural differences will change how you plan content, consent, and channels. Think of this section as a “US → Canada” pharma communications converter.

Big Picture Differences (at a glance)
| Area | United States | Canada | What to change in your workflows |
| DTC prescription promotion | Permitted with fair balance under FDA OPDP | Highly restricted; consumer-facing Rx promotions are limited (generally name/price/quantity, disease-awareness is OK without brand claims) under Health Canada advertising guidance | Split consumer vs. HCP streams; keep public content unbranded or disease-education; move brand claims behind HCP gates |
| HCP promo review | Internal MLR review; accountable to FDA standards | HCP materials commonly pre-cleared by PAAB; expected practice across industry (PAAB pre-clearance) | Add PAAB pre-clear to your Canadian promo process and timelines; version-control Canadian variants |
| Email/SMS consent | CAN-SPAM/TCPA: allow marketing with compliant opt-out/STOP | Express opt-in is the default under CASL; strict rules on implied consent and record-keeping | Use double opt-in, explicit channel scopes, and timestamped proof; suppress until consent captured |
| Privacy baseline | HIPAA Privacy Rule (plus internal policies, some state laws) | PIPEDA nationwide; provincial health-privacy acts may also apply | Keep data minimization + role-based access; be ready to fulfill access/correction requests and document lawful basis |
| Samples | PDMA: prescriber requests, receipts, lot/expiry, quantity limits | Governed by Health Canada framework and your SOPs; similar expectations on traceability and controls | Mirror U.S.-grade controls: e-sign on receipt, lot/expiry checks, inventory reconciliation |
| Transparency | Open Payments (Sunshine Act) | No national equivalent; follow internal transparency/ethical codes | Keep spend logs even without mandated public reporting; align to company code |
How to “Canadianize” a U.S. Playbook (without rebuilding everything)
Expanding north doesn’t mean rebuilding your stack. It means layering Canada-specific guardrails — think PAAB pre-clearance for HCP materials, CASL express consent for email/SMS, and a stricter stance on consumer-facing claims under Health Canada’s advertising guidance.
Below is a simple way to “Canadianize” your U.S. playbook by adjusting audiences, consent, and templates — not your entire architecture.

1) Separate your audiences by default.
Public/consumer content in Canada should be disease education or “reminder”-style (no benefit claims). Put branded claims and fair balance behind an HCP gate aligned to Health Canada’s advertising guidance, and run HCP materials through PAAB pre-clearance.
2) Make consent stricter than your U.S. baseline.
Treat CASL as “express-opt-in or don’t send.” Use double opt-in for list growth, record the scope (e.g., medical education vs. branded promotion), and enforce channel-level preferences. If you can’t prove consent, suppress.


3) Tune templates, not just copy.
Create Canadian variants of: email/SMS templates (no consumer benefit claims), web modules (HCP gating), and disclaimers (Canadian PI/monograph references). Keep them as distinct, PAAB-approved assets—don’t reuse U.S. creatives with find/replace.
4) Localize your audit trail.
Store consent proofs, pre-clearance IDs, version histories, and distribution logs specifically for Canada. If an inspector asks for “what went to Canadian HCPs in Q2,” you should export a Canada-only packet in minutes.

5) Train for the different “red lines.”
In the U.S., the line is fair balance and on-label. In Canada, the line for public content is no brand benefit claims to consumers. Reps and marketers should practice both scenarios.
Regulation Cheat Sheet (U.S. & Canada)
If that feels like information overload, don’t worry.
Use this quick reference as your pre-launch gut check:
| Topic | United States | Canada | Practical Impact |
| Promotional claims | FDA OPDP | Health Canada, PAAB | On-label only; fair balance; pre-clearance (Canada) |
| Patient privacy | HIPAA Privacy Rule | PIPEDA | Consent, minimization, access controls |
| Digital outreach | CAN-SPAM, TCPA | CASL | Express opt-in (CASL), compliant unsub/STOP, channel logs |
| Samples | PDMA | Health Canada policy (local SOPs) | Prescriber requests, receipts, lot/expiry, quantity limits |
| AE reporting | IND safety reporting | Health Canada safety reporting | Route AEs fast to safety teams; document and escalate |
| Transparency | Open Payments | (N/A national equivalent) | Aggregate HCP value transfers; public disclosures |
The 10 Most Common Failure Modes (and how to avoid them)
In practice, violations don’t come from exotic scenarios. They come from routine moments — an outdated slide, a casual phrase on a call, a missing opt-in.
Here’s where to focus your compliance audits:
Off-label creep in emails, decks, or casual call chatter. Keep to on-label, with fair balance, per FDA OPDP.
Out-of-date materials used by reps. Control access to MLR-approved content only (see Pulse Health + Veeva CLM integration).

Siloed channel data (calls in telephony, SMS in a vendor portal, emails in marketing automation) with no unified audit trail. Unify in a single system like Pulse Health.
Consent gaps (no timestamp, no scope, no proof). Align with HIPAA Privacy Rule and, for Canada, CASL + PIPEDA.
Missed or late AE routing. Use AI/keyword detection and immediate workflows; reference IND safety reporting.
PDMA violations (expired lots, over-quota, missing signatures). Build digital checks against the PDMA.

Opaque value transfers to HCPs (e.g., meals, consulting) not rolled up for Open Payments.
Audit scramble because artifacts live everywhere. Centralize records and use one-click reporting.
Unsubstantiated patient SMS/email lacking opt-out/STOP or consent audit — violating CAN-SPAM, TCPA, or CASL.
Weak access controls exposing PHI beyond need-to-know (see HIPAA Privacy Rule).
Compliance-by-Design Blueprint
People, Process, Content, Data, Channels, Monitoring
Controls work best when someone owns them. The following tips translate best practices into training, SOPs, and ownership — so compliance survives reorgs, launches, and turnover.
Here’s how to assign responsibility and cadence without slowing the work:

People: Train reps and marketers on on-label, fair balance, AE triggers, and local consent rules (U.S. vs. Canada).
Process: SOPs for MLR review, AE intake, sample handling, and escalation matrices.
Content: Only distribute MLR-approved assets. Tie distribution to platform permissions (e.g., Veeva CLM launched via Pulse Health).
Data: Capture consent + scope + timestamp; enforce minimization; implement role-based access (HIPAA/PIPEDA aligned).

Controls-to-Regulation Mapping
| Control | What it Does | Aligns To |
| Approved content library & CLM | Locks reps to latest MLR-approved assets | FDA OPDP, PAAB |
| Omnichannel logging | One patient/HCP timeline for calls, email, SMS | Audit readiness across regimes |
| Consent objects & preference center | Timestamped opt-in with channel scope | HIPAA, CASL, PIPEDA |
| AE detection & workflows | Flags AE terms, routes to safety | IND safety reporting |
| PDMA sample workflows | Digital requests, signatures, lot/expiry limits | PDMA |
| Transparency tracking | Rolls up spend/transfer-of-value | Open Payments |
| e-records & e-signatures | Integrity + audit trail | 21 CFR Part 11 principles |
Micro-SOPs You Can Deploy Tomorrow
This is the 80/20 of compliance execution. Use these bite-size procedures before launch, during engagement, and right after high-risk moments. Copy, assign an owner, and hit the ground running.
HCP Email/SMS “Pre-Flight” (U.S. & Canada)

Patient Program Outreach

- Double opt-in; clarify data use; link to privacy notice (HIPAA Privacy Rule).
- Avoid product claims; use education-first language (Canada: align to Health Canada).
- Prefer secure portals for PHI; if SMS, keep messages de-identified.
AE Capture (All Channels)
- Train teams on AE keywords and what constitutes an AE (e.g., “patient had a seizure”).
- Use AI transcription or forms to flag within the interaction.
- Auto-create an AE case; route to safety within defined SLAs (see IND safety reporting).
- Attach the original artifact (call clip, email, SMS thread) to the AE record.

PDMA-Safe Sample Handoffs
- Capture prescriber request, license verification, and digital signature on receipt (PDMA).
- Auto-check lot/expiry and quantity limits before confirmation.
- Deduct from rep inventory; surface near-expiry alerts; reconcile monthly.
Where Pulse Health Takes the Load Off
You can stitch this together with point tools — or let a platform embed the controls for you. Here’s where Pulse Health removes manual steps and hard-wires compliance into daily workflows.
- Omnichannel engagement timeline: Calls, emails, SMS, and virtual visits land on the same record with timestamps and content snapshots — see Pulse Health.
- Veeva CRM & CLM integration: Reps launch approved content in-flow so “rogue” decks never surface. Details: Pulse Health + Veeva.
- Patient messaging & partner ecosystems: Coordinate educational outreach with channel partners; for specific tactics, see Pulse Health + OptimizeRx guide and the OptimizeRx integration page.
- Consent & privacy controls: Embedded consent objects with timestamps, granular scopes, and preference centers; role-based access to protect PHI (HIPAA/PIPEDA aligned).
- AI compliance coach: Live call transcription and keyword detection (off-label phrases, AE mentions) with instant nudges and auto-routing to safety.
- PDMA sample workflows: Digital request forms, e-signatures, lot/expiry checks, and inventory reconciliation baked into the rep experience.
- One-click regulator reports: Pre-built exports for Open Payments, FDA 2253 packet support artifacts, and Canada audit logs.
- Part 11-aligned audit trails: Strong e-record integrity and user/action logs informed by 21 CFR Part 11 principles.
The simplest way to reduce findings is to reduce discretion. Pulse Health automates the risky parts so reps and marketers can focus on impact.
Implementation Roadmap (90 Days)
Big change lands better in small waves. A 90-day rollout proves value fast, locks behaviors, and surfaces gaps before you scale.

Days 0–30: Foundation
- Map channels (voice, email, SMS, portals), consent points, and sample flows.
- Import HCP/HCO account data and de-dupe; define roles/permissions (HIPAA/PIPEDA).
- Connect Pulse Health telephony/email/SMS; enable auto-logging on the HCP timeline.
- Stand up MLR content library and CLM launch via Veeva integration.
- Draft SOPs: AE intake, sample handling, content updates, and consent management.
Days 31–60: Automation & Controls
- Turn on AI transcription + red-flag detection (off-label, AE).
- Configure consent objects (scopes, geo rules, timestamps) and preference center.
- Enable PDMA workflows: request forms, e-signatures, lot/expiry validations.
- Build regulator report templates (Open Payments roll-ups, content distribution logs).
- Pilot with one BU/brand; run weekly QA on call/email samples.
Days 61–90: Scale & Optimize
- Expand to all field teams and patient programs.
- Add partner workflows (e.g., OptimizeRx integration).
- Launch dashboards (AE capture time, consent coverage, sample reconciliation rate).
- Quarterly internal audit cadence; refresh MLR content; iterate training.
KPIs That Prove Compliance (and Improve Performance)
Pick metrics that reflect control, not vanity. If you can’t audit it, don’t celebrate it.
| KPI | Target | Why It Matters |
| % interactions auto-logged to HCP record | >95% | Audit readiness; single source of truth |
| Time from AE mention → safety case creation | <24h (ideally same-day) | Meets safety expectations; reduces risk |
| % comms using approved templates/assets | 100% | Avoids off-label & outdated content |
| Consent coverage for outbound lists | 100% (by channel) | CAN-SPAM/TCPA/CASL alignment; patient trust |
| Sample reconciliation accuracy | >99% | PDMA compliance; fewer findings |
| Open Payments data completeness | 100% of reportable transfers | Transparency; avoids penalties |
| Time to assemble regulator packet | Hours → Minutes | Slashes audit/disclosure effort |

The Takeaway
Compliance isn’t a hurdle; it’s how you scale engagement responsibly. When on-label content, consent, AE capture, PDMA controls, and auditability are baked into your CRM, marketing and field teams move faster with fewer fire drills. That’s precisely why Pulse Health exists: to give pharma manufacturers a purpose-built platform where regulatory safeguards run in the background while your teams focus on outcomes.
Want to see it in action? Book a Pulse Health demo.
Or dive deeper into integrations: Pulse Health + Veeva and Pulse Health + OptimizeRx.
FAQs (For Compliance & Marketing Teams)
Yes — with consent and compliant content. Keep PHI minimal and include STOP language per TCPA and CASL. Use secure portals for anything sensitive.
Use AI support to flag risky language in real time and restrict materials to MLR-approved CLM decks (see Veeva CLM with Pulse Health).
Every handoff should have a prescriber request, license on file, digital receipt/signature, lot/expiry, and quantity logs — see PDMA.
Keep a shared core narrative, then fork for Canada: avoid DTC Rx benefits, run HCP materials via PAAB, and require CASL express opt-in for email/SMS.